They don’t.
The Department of Justice (DOJ) notes that CON laws were passed in large part because hospitals were reimbursed on a cost-plus basis, (i.e., the actual cost of care delivered). This in turn ignited a “medical arms race.” Providers lured patients to hospitals with the latest and greatest technology. Hospitals didn’t have to compete for patients based on cost – patients were insensitive to price because many were covered under generous indemnity plans at the time.
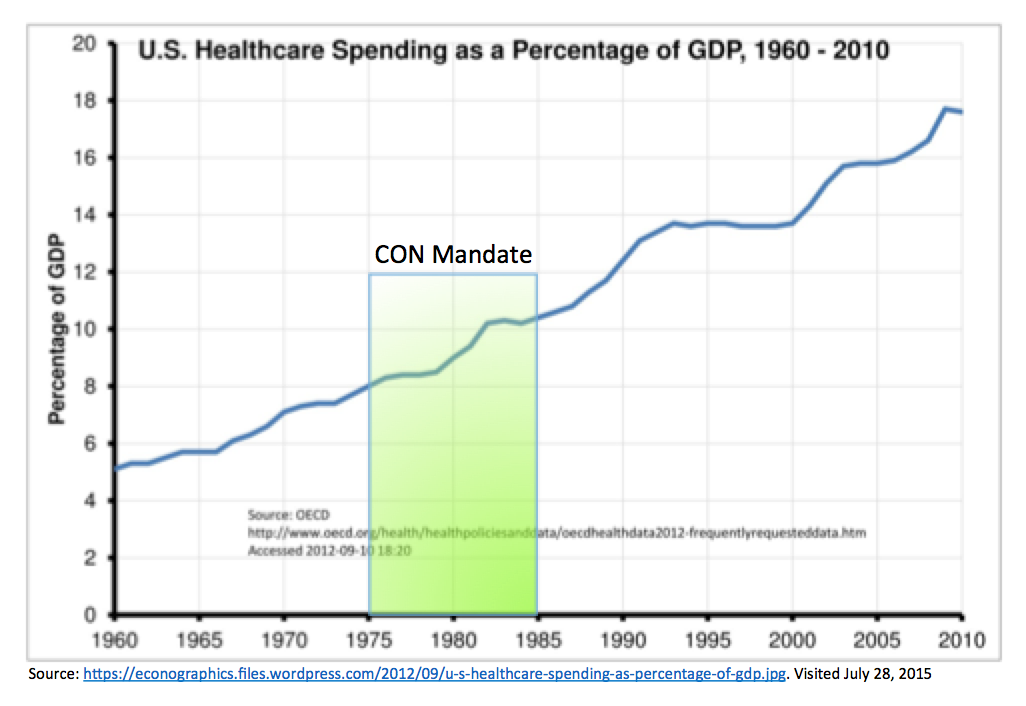
A 40-year look back shows that the federal CON mandate did not effectively slow the growth in health care expenditures. Which is why Congress repealed the mandate and made it optional for states in 1987. Just look at the chart below.
Cost containment can instead be attributed to the advent of managed care in the 1980s when insurers began to pay providers at a discounted rate in return for a guaranteed volume of patients.
Duke University’s Chris Conover and Frank Sloan conducted a widely cited study to find out whether removing CON regulations on acute care including ambulatory surgery, inpatient hospital and physician visits lead to a surge in health care spending. Controlling for factors such as other forms of regulation and area competition, the authors found that an overall surge in spending did not happen. Mature CON programs may have attributed to a 5 percent spending reduction for acute care services, but they did not constrain overall spending per-capita. Put simply, since some states’ CON programs don’t vary every service under the sun, health providers will have a tendency to acquire equipment or deliver care that isn’t regulated.
A perfect example relates to the procedure room loophole incumbent CON holders in North Carolina use to their advantage. You can read more about that here.