As Americans begin to look at the prospect of reopening businesses and restarting their economies, policymakers need to consider factors that exacerbate the spread of COVID-19. Data scientists, epidemiologists, and researchers from numerous other disciplines have created models that attempt to track the transmission of the virus before and after elected officials initiated coronavirus mitigation measures.
A working paper published by MIT economist Jeffrey Harris argues that the subway was responsible for the outbreak in New York City. CityLab described that link as “tenuous,” and a number of researchers panned the study’s methods and conclusions. Critiques of this paper focused on the presence of numerous confounding variables present in this analysis and his failure to account for transmission via other shared spaces, such as taxis, schools, restaurants, and workplaces.
North Carolina’s largest cities do not have extensive subway networks, but many do have well-developed systems of public transportation. How does the Harris hypothesis fare outside of New York City? Is there a consistent relationship between public transit ridership and COVID-19 cases in North Carolina cities? A closer look further demonstrates the dangers of making causal conclusions between the two.
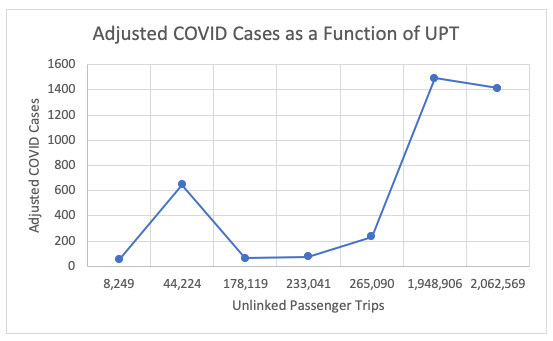
North Carolina cities with higher public transit ridership are more likely to see higher numbers of COVID-19 cases than those with lower ridership. Cities in seven metropolitan areas (Charlotte, the Research Triangle, the Triad, Fayetteville, Asheville, Wilmington, and Hickory) report unlinked passenger trips (UPT) to the Federal Transit Administration, which can serve as a proxy for the number of total people riding public transportation. The Research Triangle and the Charlotte area saw the most unlinked passenger trips (2,062,569 and 1,948,906, respectively) and the most COVID cases (1,413 and 1,494, respectively), while Hickory saw the fewest of both (8,249 and 54).
This trend holds with one notable exception: the Triad. Greensboro, High Point, and Winston-Salem have disproportionately low public transit ridership for their size (44,224). However, the COVID-19 cases there (648), while fewer than would be expected for the region’s population, are significantly higher than the expected value based on their transit ridership. This suggests that the Triad and its more populous counterparts share other underlying factors that influence COVID-19 transmission.
Cities with a higher public transit ridership likely will have higher infection rates, but it’s not known if public transportation use is the cause of transmission. For example, land use patterns and population density may create both a higher risk for COVID-19 and high public transit ridership. Alternatively, the Triad may have risk factors for COVID-19 that are not present in the other examined cities.
Is there a relationship between public transit ridership and coronavirus-related deaths in a given city? Infections do not correlate to the number of deaths, so the answer appears to be no. Other factors may actually predict mortality rate, most likely indicators of the city’s overall health. Because data regarding mortality are not sufficient, the risks of multiplying infections are unclear. Even so, minimizing infections is important at any given mortality, and the factors underlying the correlation between ridership and COVID-19 infections should be a key consideration as policymakers look to lift restrictions on businesses.
Targeted development, the high cost of automobile ownership, and the presence of denser, lower-income, and older populations all tend to be factors that lead to higher public transportation use. These may be factors that explain the anomaly of the Triad, as well as the otherwise-strong correlation between infections and ridership. Further analysis of these relationships may reveal risk factors for high infection counts, which, in turn, should inform the policies that lawmakers adopt to reopen our state.


