Health care experts are calling for more transparency in how tax dollars are being spent on physician residency programs. North Carolina ranks 5th in the nation in the amount of graduate medical education (GME) funding it receives, yet the state is an overall net importer of doctors. GME funds help teaching hospitals pay for resident salaries, benefits, and additional costs related to physician training.
“I’m going to make the argument and pitch here that simply investing in more bodies is not going to address the issue. We have to fundamentally change the way we do things,” says Dr. Erin Fraher, Director of the Program on Health Workforce Research and Policy at the University of North Carolina. Fraher and others presented data last week on the state’s physician workforce to lawmakers who sit on the graduate medical education (GME) subcommittee.
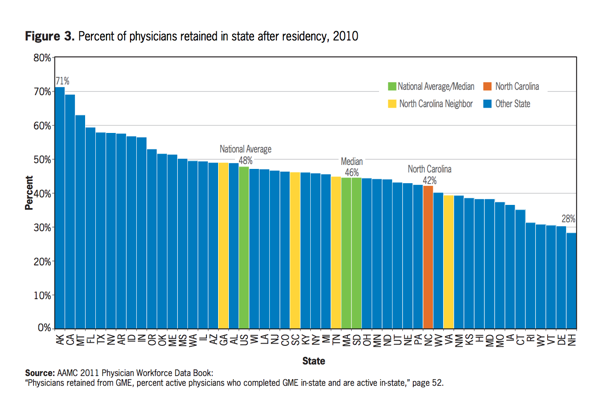
North Carolina retains just 42 percent of its physicians, and only three percent who graduated from residency programs between 2008 and 2011 are practicing in rural communities.
While the bulk of GME funds are distributed through Medicare ($9.7 billion nationwide as of 2012 data), $90 million is paid for by North Carolina Medicaid, the state-federal health program for low-income patients. Other federal GME spending comes from the Health Resources Services Administration (HRSA), and the Veterans Health Administration (VHA). Because states have more flexibility to get a better return on their investment with Medicaid GME funds, Fraher recommends that North Carolina legislators target these monies at teaching hospitals that are keeping doctors in the state. More importantly, there’s a growing consensus that all streams of GME funding should align with health care workforce demands. Under the current system, hospitals can use GME funds to open residency slots based on their own interests rather than catering to unmet patient needs.
As a result, top-down GME funding is a contributing factor to North Carolina’s physician maldistribution problem. Fraher describes it as trickle-down physician supply. Looking across North Carolina’s health care landscape, 14 percent of the state’s population live in primary care shortage areas, and 25 percent of counties don’t have a general surgeon or an OB-GYN.
“Some hospitals are good at aligning funds with workforce needs; others are not,” she says.
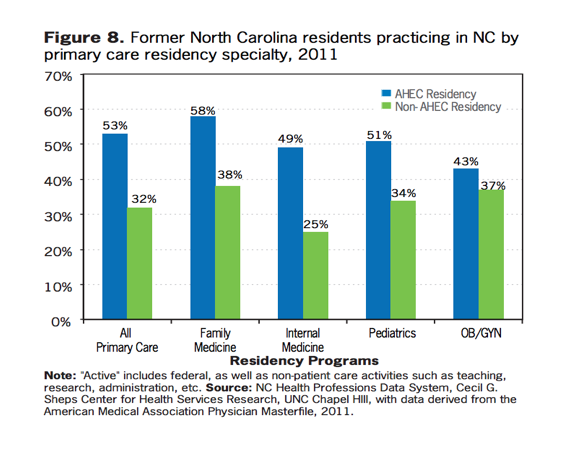
Those that are working with the state’s nine regional Area Health Education Centers (AHECs), however, are investing in opportunities for residents to train in underserved communities. Trends show that AHECs are more effective than non-AHEC residency programs at retaining physicians to practice in-state, in rural areas, and in needed specialties, like family medicine. The chart below, produced by the Cecil G. Sheps Center at the University of North Carolina, provides more context comparing in-state retention of former AHEC and non-AHEC residents by primary care specialty:
As the AHEC mission is to better match GME grants with unmet patient needs, there are more money management changes that can be accomplished by states.
Fortunately, North Carolina already has a head-start with any state-based GME reform plan it decides to pursue since the Sheps Center’s expertise is tracking where licensed health professionals locate across the state. With such a valuable resource already in place, lawmakers could create a pathway for Medicaid GME funds to follow physician trainees into the health care workforce. But for this funding stream to be more transparent, lawmakers would have to submit a waiver to the federal government asking to isolate Medicaid GME funds in a separate spending pool. The way Medicaid GME is currently calculated is complex and difficult to navigate, given that this money comes in the form of add-on payments to hospital claims and intragovernmental transfers.
If North Carolina taxpayers are going to continue paying for graduation medical education (as they have been since post-World War II), they deserve to know how exactly this money is being spent and whether it’s effectively addressing the widening rural-urban health care disparity.


