I recently blogged about the growing consensus among North Carolina lawmakers and health care experts for there to be more transparency in how state taxpayer dollars are spent on physician residency programs. North Carolina ranks 5th in the nation in the amount of graduate medical education (GME) funding it receives from Medicaid, yet the state is an overall net importer of doctors. GME funds help teaching hospitals pay for resident salaries, benefits, and additional costs related to physician training.
Right now, some states are experimenting with ways to reform how state GME funds are structured. Under the current system, teaching hospitals can use GME funds to open residency slots based on their own interests rather than catering to workforce needs.
As a result, trickle-down GME funding is a contributing factor to North Carolina’s physician maldistribution problem. Looking across North Carolina’s health care landscape, 14 percent of the state’s population live in primary care shortage areas. 25 percent of counties don’t have a general surgeon or an OB-GYN.
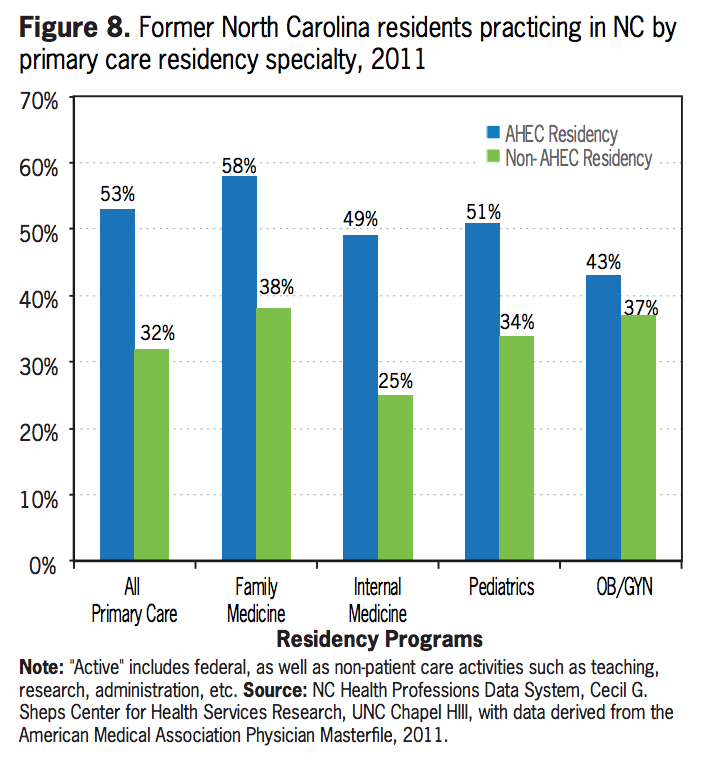
Area Health Education Centers (AHECs), however, have been instrumental in bringing better health care access to rural areas by providing opportunities for residents to train in underserved communities. Workforce trends show that AHECs are more effective than non-AHEC residency programs at retaining physicians to practice in-state, and in needed specialties, like family medicine. The chart below, produced by the Cecil G. Sheps Center at the University of North Carolina, provides more context comparing in-state retention of former AHEC and non-AHEC residents by primary care specialty:
For more information on the next steps North Carolina can take to implement GME reform, read the full Sheps Center report here.


