Local governments across North Carolina, like other employers, are wrestling with the question of how to provide quality health care to their employees in a cost-effective manner. This is particularly important for local governments because those plans are paid for by taxpayers.
One county, Union County, has piloted an innovative program in an attempt to both lower the cost of providing health care to its employees and improve the quality of, and access to, that care. In 2015, Union County expanded its health benefits to include a Direct Primary Care (DPC) option for employees.1 It is the first county in the state to offer such a plan, and its experience offers valuable lessons to other counties.
What is DPC?
Direct primary care (DPC) is a simplified health care business model that removes insurance companies from basic primary care. In exchange for a monthly, out-of-pocket fee, patients have unrestricted access to their physician and unlimited access to a defined package of services. In most cases, primary care physicians are available around the clock, in person, by phone, through text, and even via Skype. There is no limit to how often patients can access their doctors or how many services (from within the defined package) can be used. Much like a gym membership, which allows a person unrestricted access to whatever equipment and classes they wish as often as they wish, DPC grants access to whatever primary care the patient needs. And all of this is done for an average monthly fee of around $75.2,3
DPC has been around for 20 years but has only recently started to grow significantly in popularity. As of 2014, over 4,400 doctors in the U.S. had transitioned to direct primary care delivery. While this represents less than 2 percent of family doctors in the U.S., it is a significant increase from just 146 in 2005.4
As mentioned, one of the main reasons why DPC is growing is because the health care delivery model removes insurance companies from the primary care equation. By dealing directly with patients and filing no insurance billing whatsoever, DPC practices are able to eliminate 40-60 percent of their overhead expenses.5 This also frees up far more time for doctors to spend with their patients.
DPC in Union County, N.C.
Local governments, like all employers, are concerned with fulfilling the “quadruple aim,” goals generally agreed to by the health care industry6:
- Improve provider engagement
- Improve overall population health
- Enhance the patient experience
- Lower cost of care
This is what motivated Union County Human Resources Executive Director Mark Watson to consider whether DPC could be a beneficial addition to the health care options provided to the county’s employees.
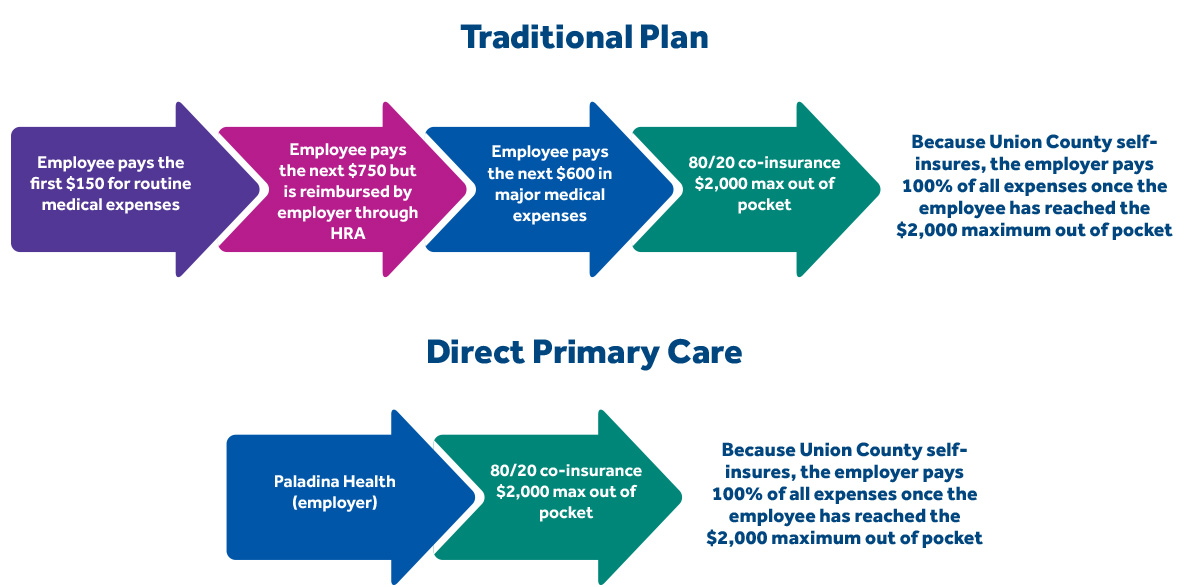
Granted, employers have been combating rising health care costs by transitioning their workers from comprehensive plans to consumer-driven health plans (CDHPs). These plans come with lower premiums and higher out-of-pocket cost sharing, and they are paired with either a tax-preferential health savings account (HSA) or health reimbursement account (HRA). The idea behind CDHPs is that when policyholders are responsible for a higher portion of out-of-pocket medical expenses, they will be more cost-conscious and shop around for the best value for health care dollars spent. Twenty-four percent of workers are enrolled in these types of plans.7
Consumer-driven plans don’t come without criticism, however. For the healthy and high-wage earners, making the switch may not be so much of a problem. But it can impose financial burdens on low-wage workers and for those who frequent the health care system.
Union County was an early adopter in providing its employees with a CDHP starting in 2003.8 Watson says that such benefit packages can yield high satisfaction rates if they are designed and managed properly. Watson and other key players then took an additional step to optimize the consumer-driven model by bringing in Paladina Health, a Direct Primary Care provider.
In April 2015, Union County added DPC to the mix, allowing employees to choose to receive their primary care services from a DPC primary care physician at a clinic set up near government offices. After the first year, results have been promising.
Patients
Perhaps the most obvious difference that patients have experienced is increased access to physicians. Same-day appointments are available, and doctors are available around the clock by phone. Those appointments are longer, allowing patients and doctors to discuss health concerns in more detail. While traditional fee-for-service appointments last seven to 10 minutes, DPC appointments average 30 to 45 minutes.9
The clinic is located near government offices, making appointments convenient. And a variety of services are available on site, including chronic disease management, fitness and nutritional coaching, vision and hearing screening, well-child visits, basic splinting and wound care, stitches, skin cyst removal, basic labs, and a variety of immunizations. On average, DPC doctors are able to provide 85 to 90 percent of patients’ health care needs. Patients are also not subject to co-pays. The membership provided by Union County covers all of these services without further fees. Under Union County’s traditional insurance plan, employees are responsible for $750 in out-of-pocket expenses for routine medical services, but that money now remains in the pockets of employees who opt for DPC.
For patients, this combination of easy access and no co-pays removes most barriers to seeing a doctor. This has been most significant for patients with chronic illnesses. According to data10,11 from Union County,
- 59 percent of DPC members have at least one chronic illness, while 35 percent are diagnosed with multiple chronic illnesses. The most common diseases are high blood pressure and hyperlipidemia.
- Of the 55 percent of DPC members in Union County who have moderate to severe chronic conditions, over 90 percent are heavily engaged with their health care. Patients with more than three chronic conditions averaged more than five visits in one year, while those with more than one chronic illness averaged over three visits.
- DPC members with more than one chronic condition cost on average 28 percent less than those enrolled in Union County’s traditional insurance plan.
Providers
DPC also looks different from the physician’s perspective. They see 70 percent fewer patients12,13 than those in traditional, insurance-based practices – eight to 10 patients per day instead of 25 to 30. This allows doctors to offer holistic primary care, reducing unnecessary specialist referrals and restoring the traditional doctor-patient relationship.
Studies show that in the traditional system of care,
43 percent of physicians spend more than one-third of their day on data entry and other administrative tasks. Other surveys say primary care physicians spend upwards of 50 percent of a patient’s office visit on the computer. Moreover, 87 percent of surveyed physicians feel professional burnout due to these administrative demands.14 Not so with DPC physicians, who can spend their days practicing medicine rather than shuffling paper. This has proven attractive and professionally satisfying to these doctors.
Employers
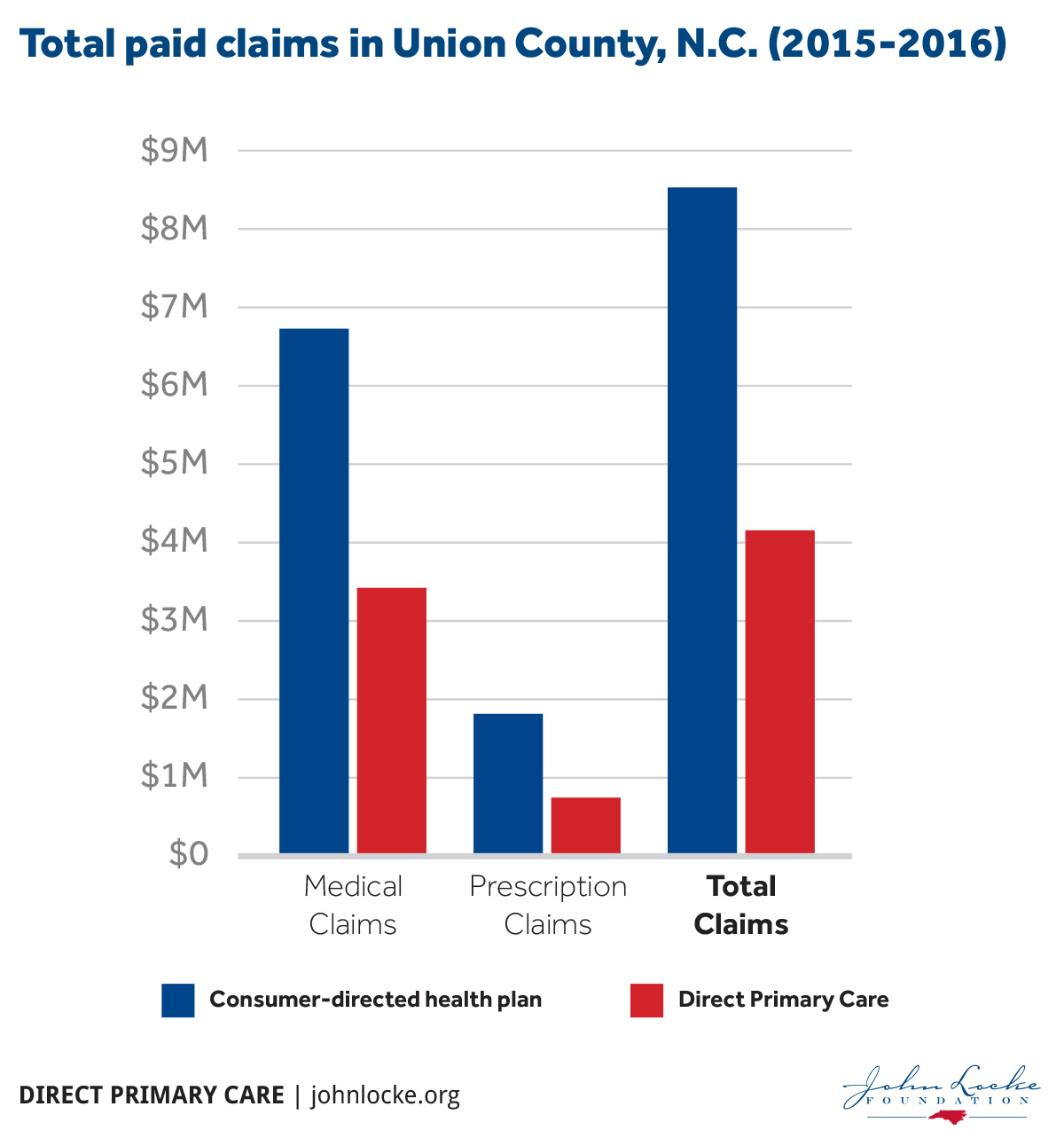
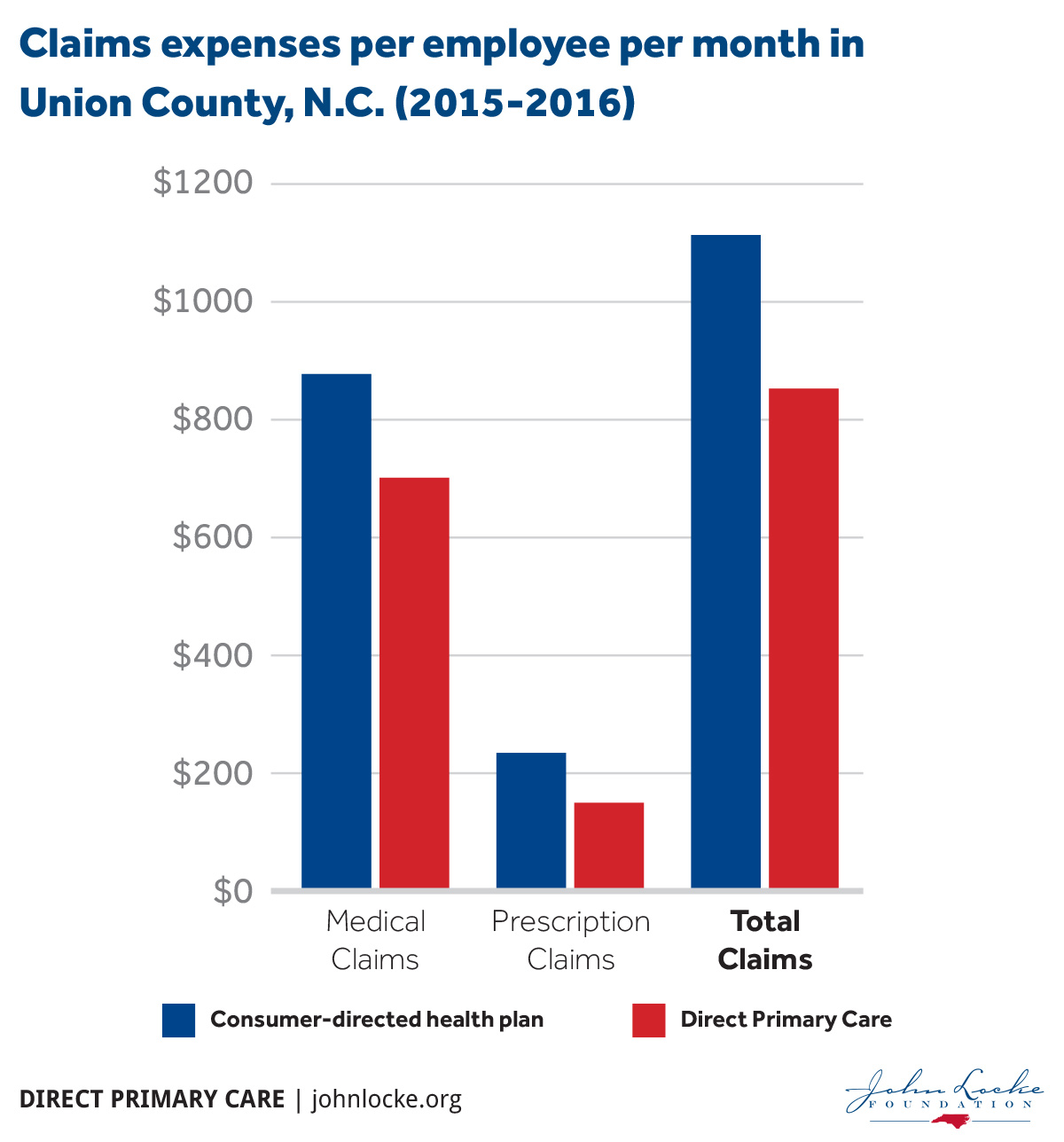
According to 2015-2016 results, DPC saved Union County, and the taxpayers who foot the bill, over $1.28 million in health care claims. This calculation is based on a comparison of the average-per-employee per month (PEPM) cost of both medical and prescription claims incurred by employees who subscribe only to Union County’s consumer-driven health plan versus those who use DPC. The previous table illustrates that the $1.28 million represents an average PEPM savings of over $260 for the 44 percent of Union County’s employees who have chosen DPC.
DPC participants
- incur 23 percent less in medical expenses than CDHP participants, yielding annual savings of $1.28 million
- incur 36 percent less in prescription expenses compared to CDHP participants, yielding annual savings of $239,000
- spend 46 percent less out-of-pocket for prescription and medical expenses than CDHP patients, a $333,639 annual savings
- report significant improvement in their overall health since electing the DPC option by a nearly 3 to 1 margin
Union County was able to implement DPC while also saving money. They did so by redirecting the $750 they were previously putting into a health reimbursement account (HRA) and using it instead to pay for a portion of the employees’ DPC memberships. This, along with claims savings, allows Union County to extend an added benefit to its employees at lower cost.
Could DPC Work Elsewhere?
Union County has about 1,000 employees. Across the state, there are more than 66,000 county government employees.15 If other counties added a DPC option, had similar employee participation rates, and accrued similar per-employee savings, statewide savings could easily amount to nearly $75 million within the first year.16 If employee participation were to increase or counties yielded larger per-employee savings, then accumulated savings would be even higher. While each county will face a unique set of circumstances, the potential savings are high enough that local governments should consider whether DPC might be a viable option for their employees.
For county governments that have tight budgets and multiple demands on limited resources, DPC offers a unique opportunity to save millions of dollars while maintaining and even improving the quality of employee health care. These are funds that could be returned to taxpayers in the form of lower property taxes or allocated to other projects that local governments wish to fund.
As health care costs continue to rise faster than the rate of general inflation,17 county government must necessarily consider new and innovative ideas. The DPC model has the potential to go beyond reforming our local and national health care delivery system and effectively transforming it.
ENDNOTES
1. Katherine Restrepo, “Union County Saves Big With Direct Primary Care.” Carolina Journal. March 15, 2016. https://www.carolinajournal.com/opinion-article/union-county-saves-big-with-direct-primary-care/
2. “DPC: An Alternative to Fee-For-Service.” American Academy of Family Physicians. 2016. http://www.aafp.org/practice-management/payment/dpc.html
3. Philip Eskew, DO, JD, MBA, and Kathleen Klink, MD, “Direct Primary Care: Practice Distribution and Cost Across the Nation.” Journal of the American Board of Family Medicine. http://www.jabfm.org/content/28/6/793.full
4. Daniel McCorry, “Direct Primary Care: An Innovative Alternative to Conventional Health Insurance.” The Heritage Foundation: Backgrounder No. 2939. Aug. 6 2014. http://www.heritage.org/research/reports/2014/08/direct-primary-care-an-innovative-alternative-to-conventional-health-insurance
5. Katherine Restrepo, “Direct Primary Care: Restoring The Physician-Patient Relationship.” Forbes. October 23, 2015. http://www.forbes.com/sites/katherinerestrepo/2015/10/23/direct-primary-care-restoring-the-doctor-patient-relationship/#54e5a77449aa
6. Thomas Bodenheimer, MD and Christine Sinsky, MD, “From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider.” Annals of Family Medicine. Vol 12 no 6 pp 573-576. http://www.annfammed.org/content/12/6/573.long
7. Employer Health Benefits 2015 Annual Survey. The Kaiser Family Foundation and Health Research and Educational Trust. 2015. http://files.kff.org/attachment/report-2015-employer-health-benefits-survey
8. Interview with Mark Watson, Executive Director of Human Resources for Union County
9. Katherine Restrepo, “Direct Primary Care: Restoring the Doctor-Patient Relatioship.” John Locke Foundation spotlight report no. 475. February 2016. https://www.johnlocke.org/research/direct-primary-care-restoring-the-doctor-patient-relationship/
10. Interview with Mark Watson, Executive Director of Human Resources for Union County
11. Katherine Restrepo, “Yes, Direct Primary Care Does Benefit Patients With Chronic Health Conditions.” Forbes. October 31, 2016 http://www.forbes.com/sites/katherinerestrepo/2016/10/31/yes-direct-primary-care-does-benefit-patients-with-chronic-health-conditions/#14b8155852f2
12. Paladina Health: Real Patients, Real Stories. 2016. https://www.paladinahealth.com/patient-stories
13. William N. Wu, Garrison Bliss, Erika B. Bliss and Larry A. Green, “A Direct Primary Care Medical Home: The Qliance Experience.” Health Affairs. vol. 29. No 5. Pp 959-962. May 2010. http://content.healthaffairs.org/content/29/5/959.extract
14. Thomas Bodenheimer, MD and Christine Sinsky, MD, “From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider.” Annals of Family Medicine. Vol 12 no 6 pp 573-576. http://www.annfammed.org/content/12/6/573.full
15. Data extraction from Union County HR Office
16. Conservative estimate based on author’s calculations
17. Mike Patton, “U.S. Health Care Costs Rise Faster Than Inflation.” Forbes. June 29, 2015 http://www.forbes.com/sites/mikepatton/2015/06/29/u-s-health-care-costs-rise-faster-than-inflation/#2f78d8cb6ad2